The Covid-19 virus required swift reaction from healthcare facilities to make changes to accommodate Covid-19 patients, from their entrances to emergency departments and ICU units. FCA’s creative design teams have been working with healthcare systems such as Weill Cornell Medicine to help them with creative ideas as a collective resource of experts on how to adapt their facilities during this global pandemic.
We asked our design team a probing question – as healthcare systems are looking back, hoping to learn from this experience, what will the focus be from their perspective on future design? This situation is impacting every facet of the healthcare system – new priorities will become clear as we begin to really understand the impact.
Healthcare workers, including the clinical team, support staff and EVS staff, will have a strong voice in how we prepare for the future. They are actively innovating on every aspect of patient care and staff safety in ways we cannot anticipate from the design professionals’ perspective. Listening and learning from them will be fascinating and challenging to the entire industry.
Healthcare workers are inventing new ways to deliver treatments, and challenging the medical equipment industry to do better. They will be demanding better diagnostic treatment and equipment. They will be pushing hospitals to provide the right PPE at the right time. They will be developing spaces that are flexible and modular that allow immediate change to accommodate burgeoning demand and impacted supply storage demands. They will be questioning infrastructure designs to be able to provide adequate ventilation and medical gases. What else will they be questioning? What are we not considering, that we cannot imagine needing – the ‘what if’ that will no longer seem so unrealistic?
The hospital administrator’s point of view will be different. With the loss of revenue for most systems occurring in the millions week to week, they will have a more critical eye on how construction dollars are spent. How do they build flexibility into their facilities to manage this influx of patients? How will ambulatory facilities be affected? We will learn soon if the COVID-19 virus re-occurs every year like the flu. Hospitals already anticipate for busy flu seasons, what will this new demand mean for increasing flexibility during this new ‘season’.
We cannot fully comprehend the impact from this virus on how healthcare spaces are designed, but we know that they will look very different. It will be a collective effort from the entire industry to ensure that the new solutions do not forget how important and impactful good interior design can be for both patients and staff.
Healthcare planning will be re-thought to make spaces safe for both staff and patients alike. There are many strategies that could be utilized to make safer healthcare spaces. The strategies should parallel the CDC’s original recommendations of distancing, washing hands, avoiding contact. Distancing and separation within healthcare facilities, re-thinking patient, staff and supply flow. Specifications of materials and surfaces that can either be easily cleaned or are anti-microbial should be considered. Leveraging technology should also be studied as a tool to design a safer facility. New facilities should consider surge design in their planning.

Lankenau Medical Center, Emergency Department, Wynnewood, Pa. Photo credit: Jeffrey Totaro
Distance / Separation
When planning for the future, it will be important to consider that any proposed solutions are not over-reactions based on the current situation, but rather creative options that are flexible and adaptable for both short term and long term solutions. Social distancing will become the norm for quite a while, and properly setting up key spaces to achieve that state will be paramount.
Healthcare entrances, including emergency department entrances, will need to be designed to take into consideration queuing that is needed with social distancing requirements for patients entering the hospital. There were long lines in hospitals that were hit hard by the virus. We can mitigate waiting outside though the design of modular elongated entry vestibules that allow for patients to queue without being exposed to the outside elements.
Additionally, exterior entrances can be designed in such a way as to extend entrance vestibules by designing new buildings, or retrofitting existing buildings to allow plastic curtains to be attached to the structure at an overhang. This would allow entrances to be extended in length in the same way that mass casualty preparation would provide tenting. Rather than utilize plastic badges or tabs that have to be cleaned in between each use, sticky labels could be printed so that the public could pull off just their label for security in hospitals. PPE stations may be considered at entrances and waiting areas.
The waiting room is where people come together, but it creates a problem for appropriate distancing. How can the amount of people waiting be minimized? There is technology that can be incorporated that provides just-in-time exam room availability, allowing for waiting rooms to be minimized. But for practices with limited budgets and access to this technology, solutions will need to be a physical response. To increase separation and distance for waiting patients and families, there will need to be less seating. The furniture will need to be designed with higher backs or screens to provide separations. A new practice might be arranged with small seating nooks distributed throughout, rather than one large space. This means there will be a need for remote visual monitoring of waiting rooms. This decentralized waiting approach will be a culture shift for best practices.
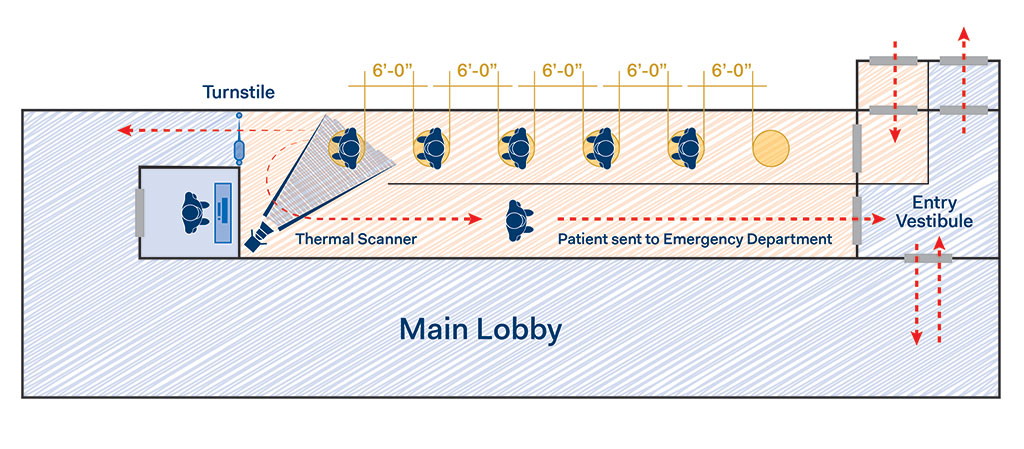
Entrance sequence diagram showing no contact thermal scanning
In the ambulatory setting, procedures will have to be assessed before a patient arrives at a facility. To limit contact with staff, check-in could happen with your phone. For those that arrive not checked-in, when a technological solution is not available, clear plexiglass screens will be needed to provide separation for reception/check-in areas, along with more space for social distancing. Converting more of the usual paperwork to a digital format will decrease the amount of materials being passed around, making one less touch point between staff and patients. We have seen the increase in tele-health reduce costs for non-emergent issues even before this pandemic. Tele-health has been crucial for enabling patients that aren’t infected to stay in touch with their physicians, but It is not an ideal solution for certain specialties such as physical therapy and radiology diagnostic testing. For these practices where in-person visits will still need to happen, we need to develop ways to still maintain safe distance and separation as much as possible.
In the hospital setting, waiting room design will also need to change post Covid-19. Social distancing will require that hospital waiting rooms have less seating, as well as more spacing between seating.

Emergency departments have been on the front lines with Covid-19 patients coming in alongside uninfected patients with a variety of other issues. Sorting out the patients with Covid-19, and keeping them away from those that are not infected has proven very difficult. In some cases, patients that came into emergency departments with Covid-19 were isolated across the hall from those without – however, the staff used the same clean and soiled rooms. Separating patients was a moot point as cross contamination occurred at the support spaces. In future designs, separate support spaces for each treatment area should be considered to prevent cross contamination.
Key to this is how patients enter and are screened. As mentioned previously, for intake triage this could mean creating a third entrance – a “fever entrance” – which will handle Covid-19 patients. The traditional walk-in vestibule will have remote biometric temperature screening. If patients have a fever of 100.4 degrees or higher they would be sent through the “fever entrance”. There would effectively be two areas in the emergency department: a regular emergency department, and a quarantine unit with isolation. Each of the quarantine areas should house a separate staff and clean/soiled utility spaces. Multi-bay treatment in these environments has been difficult, with those who are sick infecting those who are not. Care must be taken in future designs to isolate the entry sequence into the emergency department.
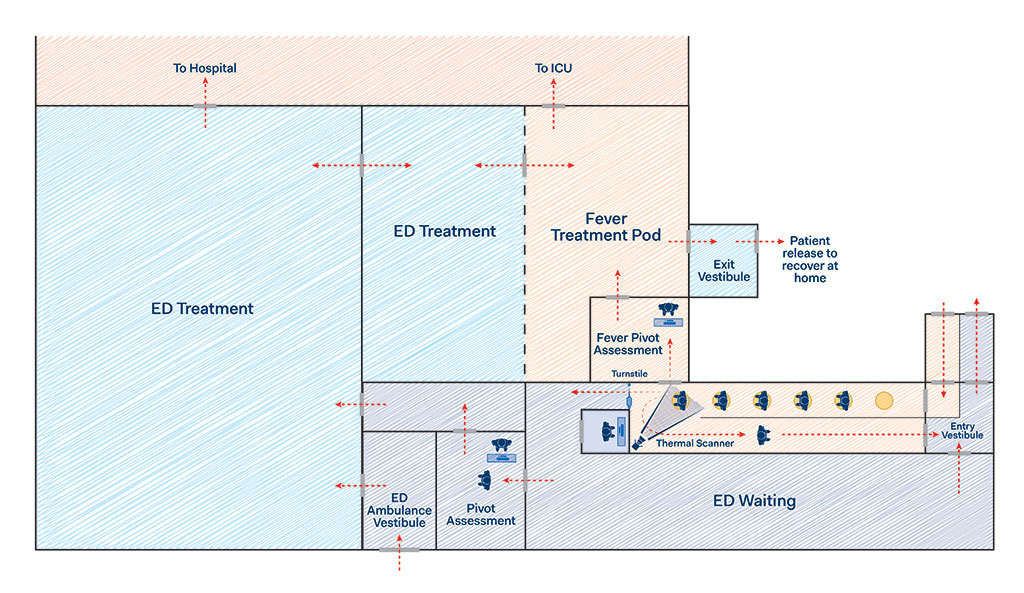
Emergency department sequence diagram
Patient, Staff and Supply Flow
The circulation of patients, staff and supplies must also be considered for distancing and separation to provide proper flow. Even though the clinical teams do interact with patients, providing off-stage staff circulation could decrease exposure. Corridors could also be widened so that a two-way flow could happen with the appropriate amount of distance.
 How the exam rooms are utilized could also be controlled.
How the exam rooms are utilized could also be controlled.
We predict that there will be a need for a higher level of cleaning that happens between patients, taking longer for rooms to be ready for the next patient. Before Covid-19, the cleaning of exam rooms between patients was limited to the exam table. Strategically using exam rooms at a 50% rate will allow for the remaining percentage to be cleaned simultaneously. Each practice will need to evaluate what makes sense for their operations. Other approaches to consider: every other exam room in a corridor could be used, or one pod or group of exam rooms could be used while another is being cleaned.
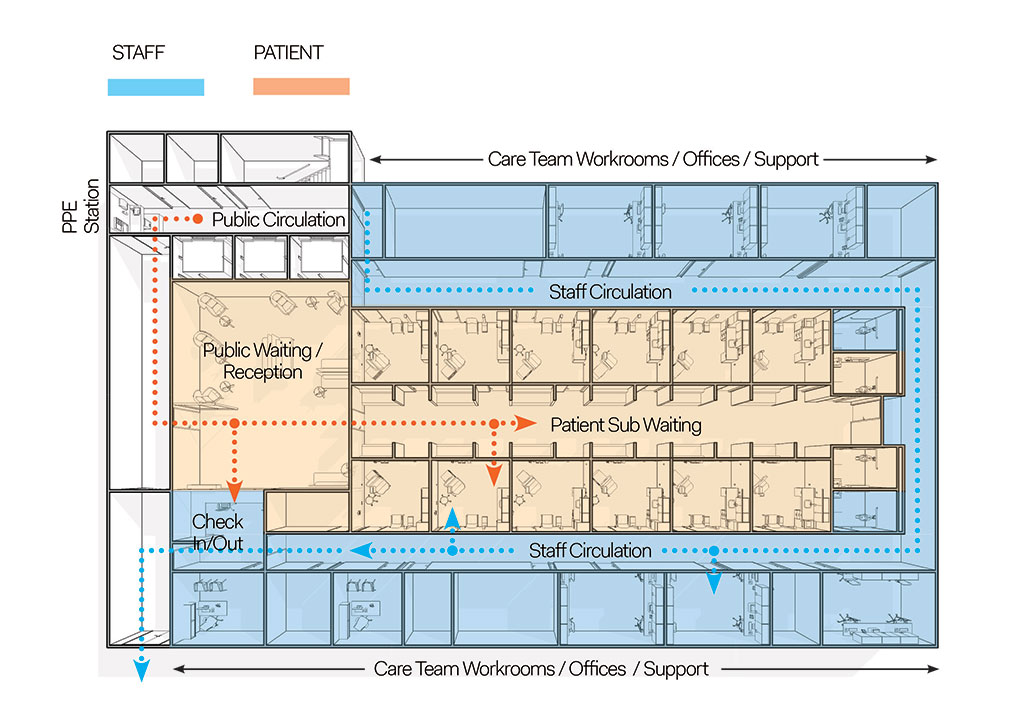
Providing off-stage staff circulation could decrease exposure
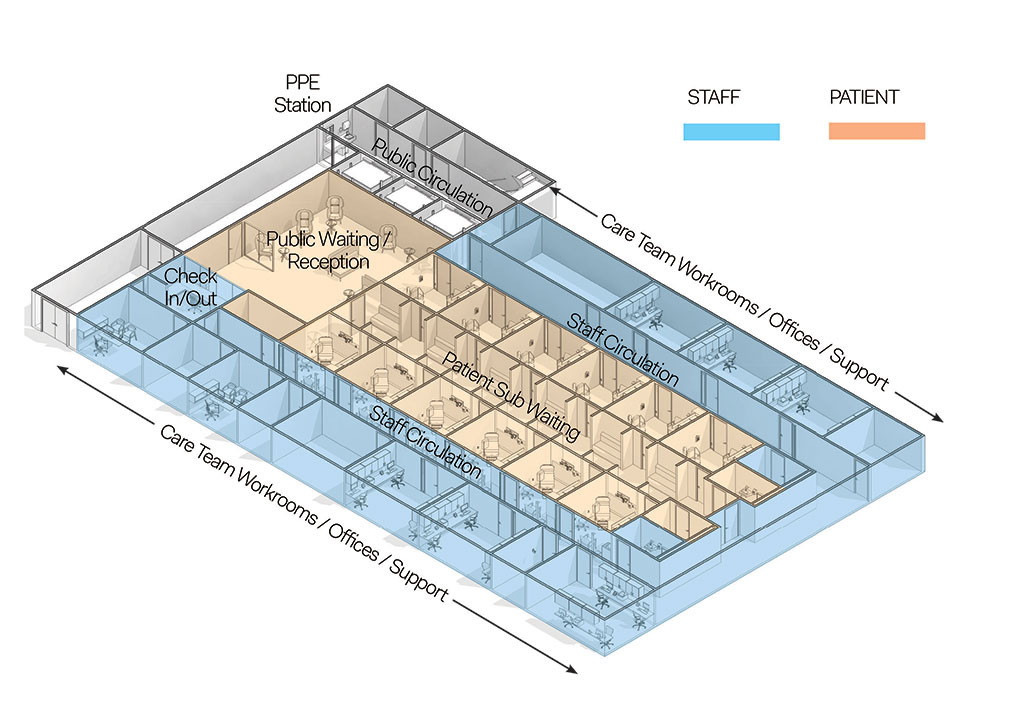
Corridors could be widened for a two-way flow with the appropriate amount of distance
Allowing more communication will be key in future design. Even if the technology is not implemented right away, it would be beneficial to provide for the infrastructure and technological backbone that would allow patients to video chat via TV or tablet. Voice controls will become more prevalent in hospitals, including elevators, patient rooms, nurse call, and alarm controls. Turning off alarms at the bedside may be a thing of the past. Nursing teams will need control outside of the room.
Materials / Surfaces
Infection control teams have always had a strong voice in healthcare interiors. They advise on cleaning protocols, and provide input on materials and cleaning methods. As the industry increases their knowledge of this virus, new cleaning protocols will be developed. Understanding materials and what they can and cannot do will be important for facilities to not overdesign and overspend. There are many products that have proven anti-microbial properties, but we will need to assess if these products are effective on the new virus. The combination of using these products with increased cleaning protocols, using new technology, will help facilities be better prepared to protect patients and healthcare workers.
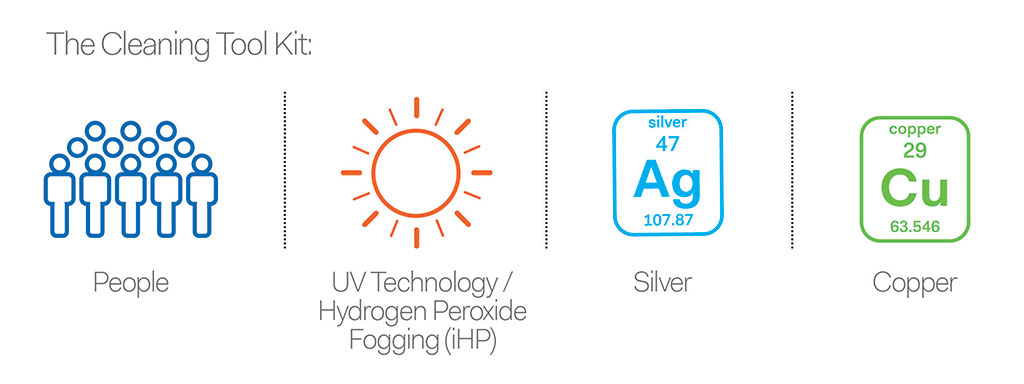
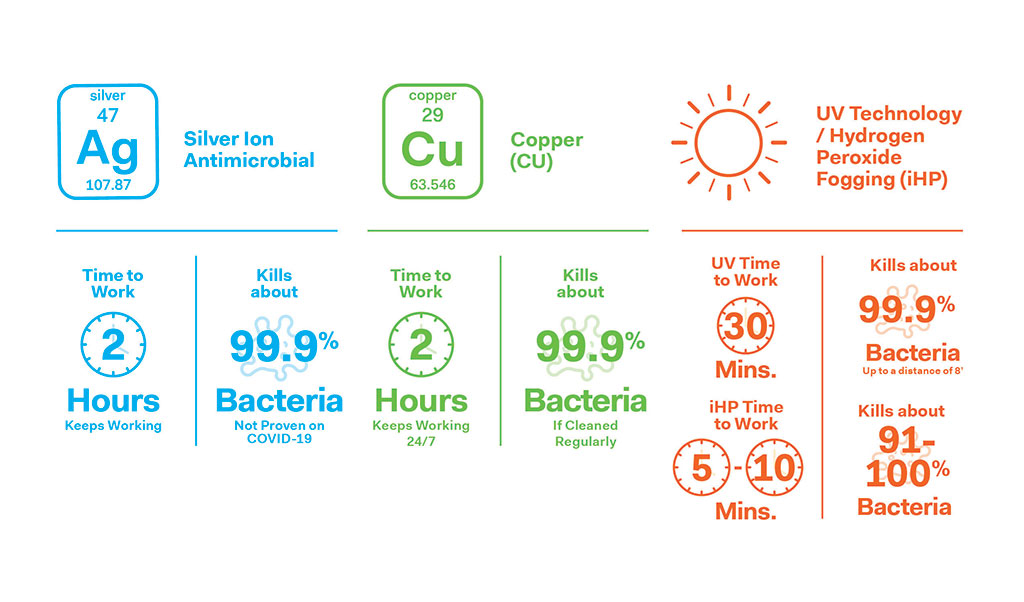
The two main areas of product development have focused around copper, its alloys, and silver. They are both known to be inherently anti-microbial. With the development of this research, and aided by the abilities of nano-technology, scientists have innovated new ways in which these naturally anti-microbial metals can be used to improve various products. Many products have been developed using this technology across all aspects of healthcare. From paints and coatings, bed rails to cubicle curtains, to hospital scrubs for staff, there are products available that embed silver or copper molecules to help kill bacteria. There have been research studies that prove their effectiveness, killing bacteria in 2 hours and continuing to work 24/7 (with some caveats). A quick web search will provide a lot of information. As with anything, we need to read and be aware of the pros and cons of these products. Silver and copper products work differently, are made differently, and are added to products in different and various ways. As new products are developed, specifiers need to be aware of these differences to ensure that they are not creating health hazards in their production. Not all products are equal, and efficacy varies from product to product depending on how they are manufactured. There is an ongoing debate as to the overuse of nanosilver in products in general. Will humans build up a resistance to silver? Should we reserve its use for more severe healthcare uses, to continue to protect against superbugs? Similarly with copper, overselling its properties can occur, and some items might have no effect. The design industry has made in-roads towards developing an understanding of the cradle-to-cradle impact of products on our world and on human health. We need to maintain that rigor to not lose ground in continuing to create healthy environments.
 The industry is going to have to evaluate new cleaning strategies that make sense, and that can be maintained over time. They will need to be evident to the public, so they have confidence in their safety while visiting these spaces. Interior designers use various strategies to prompt safe habits in healthcare environments. They are there to nudge and remind clinical teams to maintain appropriate safety standards. Handwash locations have been designed with different colors on both the walls and floors, so that they stand out as a reminder for clinical teams to wash their hands. There have also been floor and wall prompts at medication prep stations to remind staff to not disturb other staff while they are working with medications for patients. These interventions have been successful in lowering medication errors and HAI’s (“hospital-acquired infections”). This approach to encourage safe habits will have to be rolled out with a more outward public approach. For example, we can use these strategies to indicate PPE locations, and to indicate safe distances in corridors and circulation paths within suites. Changes in flooring color or finish will help to denote appropriate social distancing space requirements for patients and staff.
The industry is going to have to evaluate new cleaning strategies that make sense, and that can be maintained over time. They will need to be evident to the public, so they have confidence in their safety while visiting these spaces. Interior designers use various strategies to prompt safe habits in healthcare environments. They are there to nudge and remind clinical teams to maintain appropriate safety standards. Handwash locations have been designed with different colors on both the walls and floors, so that they stand out as a reminder for clinical teams to wash their hands. There have also been floor and wall prompts at medication prep stations to remind staff to not disturb other staff while they are working with medications for patients. These interventions have been successful in lowering medication errors and HAI’s (“hospital-acquired infections”). This approach to encourage safe habits will have to be rolled out with a more outward public approach. For example, we can use these strategies to indicate PPE locations, and to indicate safe distances in corridors and circulation paths within suites. Changes in flooring color or finish will help to denote appropriate social distancing space requirements for patients and staff.
Reducing physical contact of surfaces is another great way to limit exposures to germs. When we focus on healthcare spaces and how many items are touched at every patient visit, we can begin to discuss how to limit contact with these items. For example, clinical teams touch cabinets, sinks, trash cans, soap dispensers, paper towel dispensers, and glove dispensers in an exam room. Increasing the use of hands-free devices on doors, plumbing fixtures and other high-touch items can reduce exposure and can minimize the items that need to be wiped down in between each patient. Changing protocols within these spaces can be reinforced with visual cues such as colors, graphics and text. By having these protocols stand out obviously to patients, they will feel more comfortable maintaining their visits, which will ultimately keep them healthy.
Environmental service teams are crucial to successful healthcare environment protocols. Providing them the appropriate protections for themselves, and the correct tools and training to meet the demands of their work is imperative. Without them, any efforts to keep our environment clean will break down.
Implementing new technologies is another strategy to add to the arsenal of tools. There are two techniques that have come into focus recently. They have both been used in various other industries, but with the Covid -19 infections, are being leveraged at a greater rate to help with keeping facilities clean. Both UV Light technology and Hydrogen Peroxide Fogging(iHP) should be considered as a way to decrease pathogens within health care settings. Understanding what each device can do is important. UV light’s effectiveness is dependent on the proximity of the surface to the lamps. The light does not penetrate, so the intended surface must be exposed to the light for it to be effective. UV technology, in partnership with a good systematic cleaning policy, can be effective in minimizing bacteria on surfaces.
Hydrogen Peroxide Fogging(iHP) is a fast way to blast surfaces, the process can get into the nooks and crannies that can be overlooked when a person cleans a space. It works very fast, killing most bacteria within minutes.
Silver Ion Antimicrobial
Time to work: 2 hours (keeps working)
Effectiveness: Kills about 99.99% bacteria (not proven on COVID-19)
How it works
- Positively charged silver ions and negatively charged microbe cells are attracted to each other upon contact.
- Silver ions pierce through the external surfaces of the cells and damage their DNA, as well as the protein structure, halting their metabolism and reproduction until they die. This explains the sterilization effect of silver ions.
- After the cells have become inactive, silver ions leave but continue to act against microbes, delivering a constant antimicrobial performance with no toxicity or side effects.
Copper (CU)
Time to work: 2 hours (keeps working 24/7)
Effectiveness: Kills about 99.99% bacteria if cleaned regularly
How it works
- It disrupts bacterial cell membranes — copper ions damage cell membranes or “envelopes” and can destroy the DNA or RNA of the microbe.
- It generates oxidative stress on bacterial cells and creates hydrogen peroxide that can kill the cell.
- It interferes with proteins that operate important functions that keep bacterial cells alive.
Continues working 24/7, kills 99.9% of certain bacteria if cleaned regularly, copper can be effective against SARS-CoV-2.
The study showed that after four hours, the virus was no longer infectious on copper’s surface. In comparison, coronavirus was still infectious on plastic surfaces after 72 hours.
UV Technology / Hydrogen Peroxide Fogging (iHP)
UV time to work: 30 mins
UV effectiveness: Kills about 99.99% bacteria up to a distance of 8’
iHP time to work: 5-10 mins
iHP effectiveness: Kills 91-100% bacteria
How it works
- UV light can have efficient inactivation of bacteria up to a distance of eight feet on either side, and exposure time of 30 minutes is adequate.
Disadvantage: The radiation is not very penetrating, so the organism to be killed must be directly exposed to the rays. Another potential problem is that UV light can damage human eyes, and prolonged exposure can cause burns and skin cancer in humans.
Distance from surfaces and angle of incidence are two of the most important factors influencing UV-C efficacy.
“Hydrogen peroxide oxidizes the walls exposing the nuclei, and kills it on contact. One advantage of iHP, therefore, is the active manner and speed with which the mist droplets are dispersed to surfaces.”
Disadvantages: Liquids and vapors, such as hydrogen peroxide, are limited by temperature and environmental factors which can alter their effectiveness.
Credits:
New England Journal of Medicine
www.ncbi.nlm.nih.gov/pmc/articles/PMC6315945/
www.smithsonianmag.com/science-nature/copper-virus-kill-180974655/
www.insider.com/does-copper-kill-germs-and-viruses
www.infectioncontroltoday.com/environmental-hygiene/fast-track-zero-environmental-pathogens-using-novel-ionized-hydrogen-peroxide
Smart Technology
Smart technology continues to impact so many activities in our daily lives, we will see more and more technology integrated into visits to healthcare environments. Telemedicine has taken a front seat in this pandemic, and its importance has changed forever. From family practice to specialists, clinical care teams are using digital appointments to accommodate their patients during this crisis. Telemedicine has also aided in the monitoring of ICU patient rooms. New unit design should consider including cameras that are observed from nursing stations, not only in ICU units but also in regular medical/surgical units. Telemedicine can also provide distancing and connectivity so that clinicians can observe patients outside of their rooms. Home care will be changing as wearables will take on new importance. At many hospitals, patients are being discharged with portable pulse oximeters to monitor oxygen levels. Early reports coming out of China and Italy, two areas where COVID-19 took hold earlier in the pandemic, show that up to 1 in 5 patients with the illness end up with heart damage. Patients who were on ventilators might be utilizing mobile EKG heart monitors to track long-term damage. (Source: Johns Hopkins.)
Electronic medical records have changed the way both physicians and patients deal with each other. The larger health systems have adopted them across platforms more than smaller, suburban health systems. They are expensive to roll out — software, hardware, and training all take time and resources. Even larger health systems have taken years to get entire healthcare systems up and running. The new attitude towards preparing for the unknown will make increasing our reliance on technology even greater. With this increased need, technology companies will have a part to play in developing products that are more available to a wider audience.
Having to sign-in on paper clipboards should be a thing of the past. With a larger part of the population having access to mobile phones, geo-tracking software could be used to check patients in and out, notify arrivals at physician practices and provide directions on where to go upon arrival. Why not proceed directly to an exam room? Patients could check-in online and guide themselves to their exam room. The path of travel could have auto-open doors all the way to the exam rooms.
Having real time information can help the bottom line too. Reducing sizes of waiting rooms could decrease the size of real estate needed. With effective administrative processes and room turn-around time, more patients could be seen in a typical day. With the shortage of physicians and nurses, leveraging their time using technology can provide more access to healthcare.
Surge Design
Healthcare institutions have been stretched to accommodate the surge of Covid-19 infected patients requiring ventilators and ICU levels of care. As new medical/surgical patient units are designed, consideration should be given for surge design and for providing future flexibility to create Acuity adaptable plans with remote servers and ante-rooms or alcoves to house sicker patients needing ventilators and ICU care. New units that are designed in this manner would allow regular patient units to flip over to accommodate infectious disease patients faster and more efficiently. All the required needs for an ICU level room would be included in this med/surg room, such as medical gases, regular and emergency outlets, patient monitoring and code-mandated mechanical requirements. Working with your engineering partners to create options that allow for easy switch over to higher levels of HEPA filtration and pressurization changes needed in the rooms.
In these new patient units, space is needed to quickly convert regular patient rooms into ICU level rooms. PPE donning and doffing should be considered at the entrance of each unit. Space should be defined to allow an ante room either permanently or temporarily set up, and portable and collapsible vestibules that are needed to seal off rooms so that disease does not escape. Typically, hallways are 8’-0” in width for stretcher movement. Hallways of the future will need to look at that dimensions with a critical eye, and allow for space for the ante room as well as space to remove all unnecessary equipment to storage just outside the room. We suggest that this space be developed outside of the clear 8’-0” traffic zone to allow for maximizing the space.

Acuity adaptable unit in normal condition
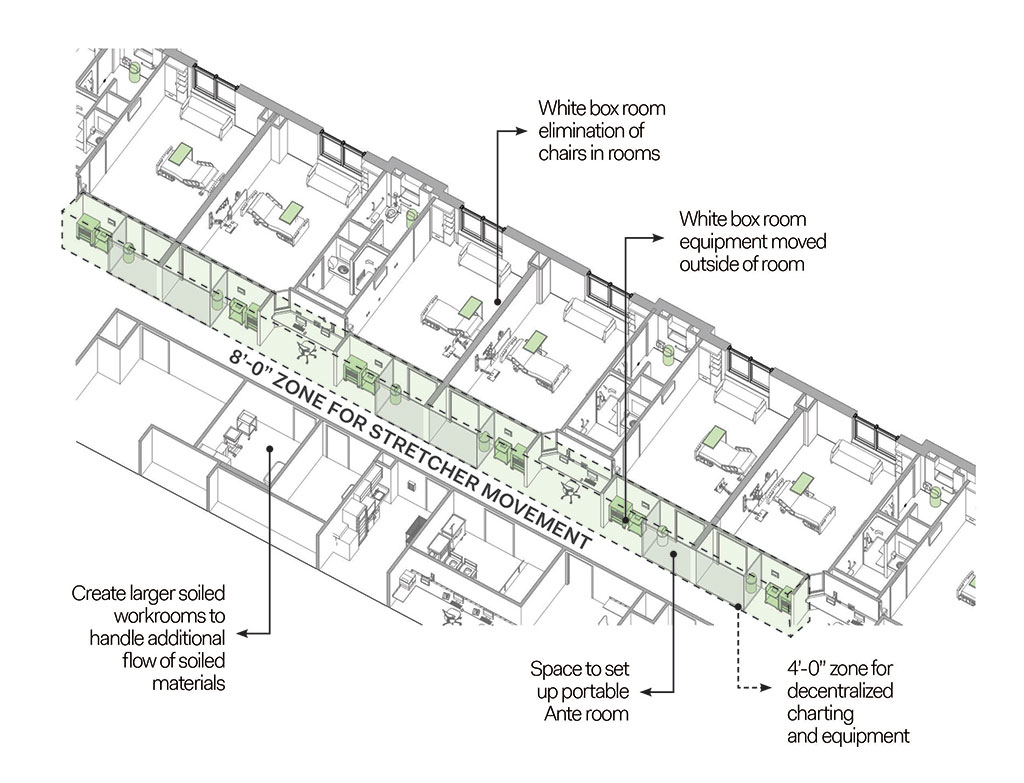
Acuity adaptable unit in surge condition
During the pandemic, hospitals were turning prep and recovery spaces for operating rooms and cath labs dedicated to elective use into Covid-19 treatment areas. Looking at the future design of these types of spaces, planning will not only accommodate their proposed use but each will have a unique strategy to allow a seamless accommodation for the treatment of infectious patients if needed. Ventilation, medical gases, and normal and emergency outlets should be considered when designing these prep/recovery spaces.
About the authors

Catherine Gow
Principal, Health Facilities Planning
FCA
Catherine Gow is the Principal of FCA’s healthcare planning practice. Her more than 20 years of experience in healthcare planning has included master plans, system consolidation planning, and department planning for complex areas such as emergency departments, surgery and imaging suites, cardiac care, cancer centers and critical care units. Catherine’s work has been highlighted in publications such as Healthcare Design and Health Facilities Management, and has achieved honors such as the 2010 ASHE Vista Award for New Construction. She is a member of the American Institute of Architects (AIA), ASHE, NCARB, and is Lean Six Sigma certified.
 Jennifer Kenson
Jennifer Kenson
Principal, Interior Design
FCA
Jennifer Kenson, Principal of Interior Design for FCA, has been creating successful interior environments for over 20 years. Her experience extends not only to planning and interior architecture, but also interior materials and finishes. Her writing has appeared in publications such as Healthcare Design, Interiors and Sources and Medical Construction and Design, and her projects have received awards from the Healthcare Facilities Symposium and General Building Contractors Association, among others. She is a member of the International Interior Design Association (IIDA) and NCIDQ, and is Lean Six Sigma certified.